
1
WHO global lists of
high burden countries for
tuberculosis (TB), TB/HIV and
multidrug/rifampicin-resistant
TB (MDR/RR-TB),
2021–2025
Background document
WHO global lists of high burden countries for TB, multidrug/rifampicin-resistant TB (MDR/RR-TB) and
TB/HIV, 2021–2025
ISBN 978-92-4-002943-9 (electronic version)
ISBN 978-92-4-002944-6 (print version)
© World Health Organization 2021
Some rights reserved. This work is available under the Creative Commons Attribution-NonCommercial-
ShareAlike 3.0 IGO licence (CC BY-NC-SA 3.0 IGO; https://creativecommons.org/licenses/by-nc-
sa/3.0/igo).
Under the terms of this licence, you may copy, redistribute and adapt the work for non-commercial
purposes, provided the work is appropriately cited, as indicated below. In any use of this work, there should
be no suggestion that WHO endorses any specific organization, products or services. The use of the WHO
logo is not permitted. If you adapt the work, then you must license your work under the same or equivalent
Creative Commons licence. If you create a translation of this work, you should add the following disclaimer
along with the suggested citation: “This translation was not created by the World Health Organization
(WHO). WHO is not responsible for the content or accuracy of this translation. The original English edition
shall be the binding and authentic edition”.
Any mediation relating to disputes arising under the licence shall be conducted in accordance with the
mediation rules of the World Intellectual Property Organization
(http://www.wipo.int/amc/en/mediation/rules/).
Suggested citation. WHO global lists of high burden countries for TB, multidrug/rifampicin-resistant TB
(MDR/RR-TB) and TB/HIV, 2021–2025. Geneva: World Health Organization; 2021. Licence: CC BY-NC-
SA 3.0 IGO.
Cataloguing-in-Publication (CIP) data. CIP data are available at http://apps.who.int/iris.
Sales, rights and licensing. To purchase WHO publications, see http://apps.who.int/bookorders. To submit
requests for commercial use and queries on rights and licensing, see http://www.who.int/about/licensing.
Third-party materials. If you wish to reuse material from this work that is attributed to a third party, such
as tables, figures or images, it is your responsibility to determine whether permission is needed for that reuse
and to obtain permission from the copyright holder. The risk of claims resulting from infringement of any
third-party-owned component in the work rests solely with the user.
General disclaimers. The designations employed and the presentation of the material in this publication do
not imply the expression of any opinion whatsoever on the part of WHO concerning the legal status of any
country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or
boundaries. Dotted and dashed lines on maps represent approximate border lines for which there may not yet
be full agreement.
The mention of specific companies or of certain manufacturers’ products does not imply that they are
endorsed or recommended by WHO in preference to others of a similar nature that are not mentioned. Errors
and omissions excepted, the names of proprietary products are distinguished by initial capital letters.
All reasonable precautions have been taken by WHO to verify the information contained in this publication.
However, the published material is being distributed without warranty of any kind, either expressed or
implied. The responsibility for the interpretation and use of the material lies with the reader. In no event
shall WHO be liable for damages arising from its use.

1
Introduction
During the period 1998 to 2015, the concept of a “high burden country” (HBC) became familiar and widely
used in the context of tuberculosis (TB). The first global list developed by WHO consisted of 22 HBCs with
approximately 80% of the world’s TB cases; this was established in 1998. Subsequently two other HBC lists,
for HIV-associated TB and multidrug-resistant TB (MDR-TB), were defined.
In 2015, three WHO global lists of HBCs – for TB, TB/HIV and MDR-TB - were in use. With a new era of
the Sustainable Development Goals and the End TB Strategy starting in 2016, a thorough review of these
three global HBC lists was undertaken by the WHO Global TB Programme in 2015.
1
This included
consideration of whether the lists should be modified (and if so how) or whether they should be discontinued.
The outcome of the review was the definition of three new global HBC lists for the period 2016–2020: one
for TB, one for TB/HIV and one for MDR-TB. It was also agreed that these lists would be reviewed again
in 2020.
This background document is about the global HBC lists to be used by WHO from 2021–2025. It is
structured in four main parts. The first summarizes the review undertaken in 2015, including the process, the
main findings from consultations with stakeholders and the recommendations of WHO’s Strategic and
Technical Advisory Group for TB (STAG-TB). The second describes the three global HBC lists that were
defined by WHO for 2016–2020. The third explains the updated global lists to be used for the period 2021–
2025; these have been defined using the same criteria as those agreed in 2015, in combination with the most
recent estimates (for 2019) of the incidence of TB, HIV-associated TB and MDR/rifampicin-resistant TB
(MDR/RR-TB)
2
that were published in WHO’s Global Tuberculosis Report 2020. Entries to and exits from
the current lists are highlighted. The fourth section highlights how regional priority lists can complement the
three global HBC lists.
1. Review in 2015 that resulted in three new WHO global lists of HBCs for 2016–2020
The WHO Global TB Programme prepared a discussion document on global HBC lists in April 2015. This
was circulated across the WHO TB network (HQ, regional and country offices) and to a range of external
partner agencies for feedback. An online survey to elicit input from a wide range of stakeholders was run for
two weeks in May 2015; this was completed by 323 people, of which 50% were national respondents
(national TB programmes, national nongovernmental organizations, civil society representatives, national
Ministries of Health or public health agencies) and 34% were respondents from international or technical
agencies. The remaining 16% identified themselves as in an “other” category. An updated version of the
discussion document and an accompanying presentation were then prepared for consideration at the June
2015 meeting of WHO’s STAG-TB.
Main findings from stakeholder consultations in 2015
The main findings about whether WHO should continue to use global HBC lists, and their associated
advantages and disadvantages, were:
1. There was strong support for continuing the use of global HBC lists. Only 5% of respondents
preferred the option of stopping the use of global HBC lists, and none of these respondents was from
a national constituency.
2. There was strong agreement that global HBC lists are important to help national TB programmes in
HBCs to advocate for political commitment (including funding) from their own governments as well
as international funding agencies. This was true overall and for all constituencies.
3. There was strong agreement that global HBC lists are important to prioritize international donor
funding and technical assistance for countries where improving TB prevention, diagnosis and
treatment is most needed to have a global impact. This was true overall and for all constituencies.
1
Use of high burden country lists for TB by WHO in the post-2015 era. Discussion paper initially prepared in April 2015 to
facilitate feedback, and finalized after the June 2015 meeting of WHO’s Strategic and Technical Advisory Group for TB (STAG-
TB). Available at: https://www.who.int/tb/publications/global_report/high_tb_burdencountrylists2016-2020.pdf
2
The lists for 2016–2020 were based on the incidence of MDR-TB (i.e. resistance to both isoniazid and rifampicin). Since 2016,
following updates to treatment guidelines, WHO has focused on estimates of the incidence of rifampicin-resistant TB, which
includes MDR-TB, and referred to these as estimates of MDR/RR-TB. About 80% of people with RR-TB have MDR-TB.

2
4. There was strong agreement that global HBC lists are important to ensure that countries with a
serious TB, TB/HIV or MDR-TB problem are included in the priority lists of international and
technical agencies. This was true overall and for all constituencies.
5. There was agreement (most respondents agreed or strongly agreed, with more in the former category)
that global HBC lists encourage global and regional monitoring in a consistent set of countries.
6. There was either strong agreement or agreement that countries not in the global HBC lists in use in
2015 may have been relatively neglected by international funding and technical agencies, even when
they had a high burden relative to population.
The main findings related to the future design of global HBC lists were:
1. The preferred option was to develop 3 new lists based on new criteria (about 50% of respondents).
About 40% favoured updating the lists using the original criteria, and about 15% favoured the
development of one list only.
2. The vast majority (about 80%) of respondents favoured lists of between 11 and 30 countries. The
remaining 20% were approximately split between a list of 10 or fewer countries, and a list of more
than 30 countries.
3. The vast majority (about 85%) of respondents favoured lists that have a lifetime of 3–5 years.
4. The lists should be defined using consistent criteria and have consistent cut-offs in terms of the share
of global burden accounted for by the countries in each list.
5. Lists should be defined not only on the basis of a country’s absolute number of TB cases but should
also include countries with a severe TB burden (e.g. in terms of incidence per 100 000 population
per year).
Proposal presented by GTB at the WHO STAG-TB meeting in 2015
Based on feedback from stakeholder consultations, one proposal for three new global HBC lists for the period
2016–2020 was presented by GTB for consideration by WHO’s STAG-TB in June 2015.
The proposed lists were defined based on the following principles/design characteristics:
1. The purpose of each list should be stated.
2. The lists (TB, MDR-TB, TB/HIV) should be defined using consistent criteria.
3. The lists should result in similar cut-offs in terms of the share of the global burden accounted for
by the countries in the list.
4. The criteria used to define lists should be easy to explain, use and reproduce.
5. The time period (useful life) of the list should be defined.
6. The list should be relatively short (no more than 30 countries).
7. If possible, there should be a clear distinction between countries in and outside the list.
The proposed global lists were characterized as three “20+10” HBC lists: one for each of TB, MDR-TB and
TB/HIV, that would have a lifetime of 5 years. Each list included 30 countries, consistently defined as the
top 20 in terms of their estimated absolute number of incident cases per year, plus the 10 countries with the
most severe burden (e.g. in terms of incidence per 100 000 population per year) that do not already appear
in the top 20 (“20+10”).
3
The proposed lists resulted in similar cut-offs (85–89% of the estimated global
burden). The lists could be reproduced by anyone based on incidence estimates (for TB, HIV-associated TB
and MDR/rifampicin-resistant TB) published in WHO’s annual global TB report. The purpose of each list
was clearly stated, and in a consistent way for each list. For example, the purpose of the TB list was defined
as:
“To provide a focus for global action on TB in the countries where progress is most needed to
achieve End TB Strategy and SDG targets and milestones, to help build and sustain national political
commitment and funding in the countries with the highest burden in terms of absolute numbers or
severity, and to promote global monitoring of progress in a well-defined set of countries.”
3
STAG-TB members were also asked for their suggestions, if any, regarding one consolidated list. Their comments were that the
diagram shown on page 3 of this document illustrated why it would be better to have three separate lists, rather than attempting to
develop one consolidated list.
3
WHO STAG-TB comments and recommendations in 2015
The comments and recommendations at the June 2015 meeting of WHO’s STAG-TB were summarized in
the meeting report
4
as follows:
“STAG-TB:
• Recognizes the value of high TB burden country (HBC) lists;
• Supports the proposal for WHO to use three “20+10” HBC lists (TB, MDR-TB, TB/HIV) post-
2015, which will have a lifetime of 5 years.
STAG-TB recommends that WHO:
• Define the additional 10 countries in all three lists using rates (as opposed to the alternative option
of using proportions of cases with HIV co-infection or MDR-TB for the TB/HIV and MDR-TB
lists);
• At Regional Office level, consider whether to develop more extended regional lists of HBCs, using
consistent methods.”
For countries included in lists based on their estimated incidence per 100 000 population per year, STAG-
TB also recommended the application of a threshold for a minimum number of cases, to avoid global lists
including countries with very small numbers of cases that would fit better within regional HBC lists.
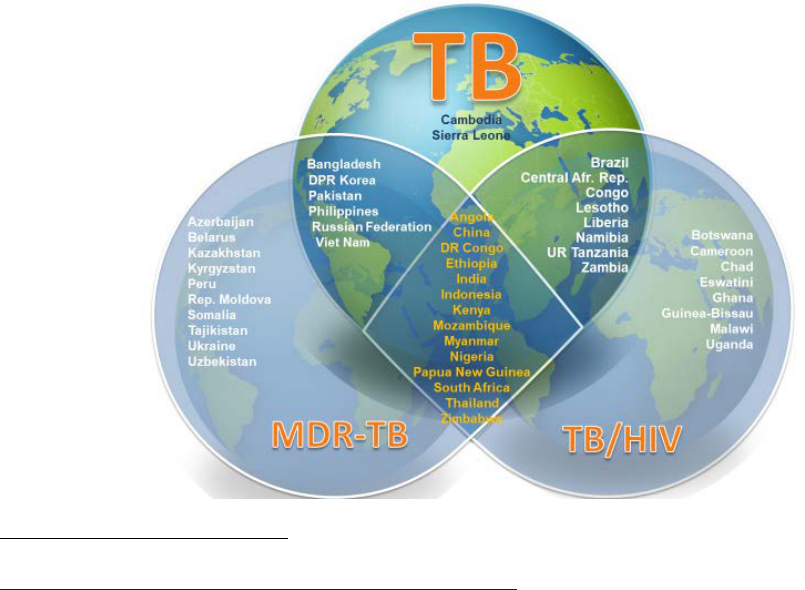
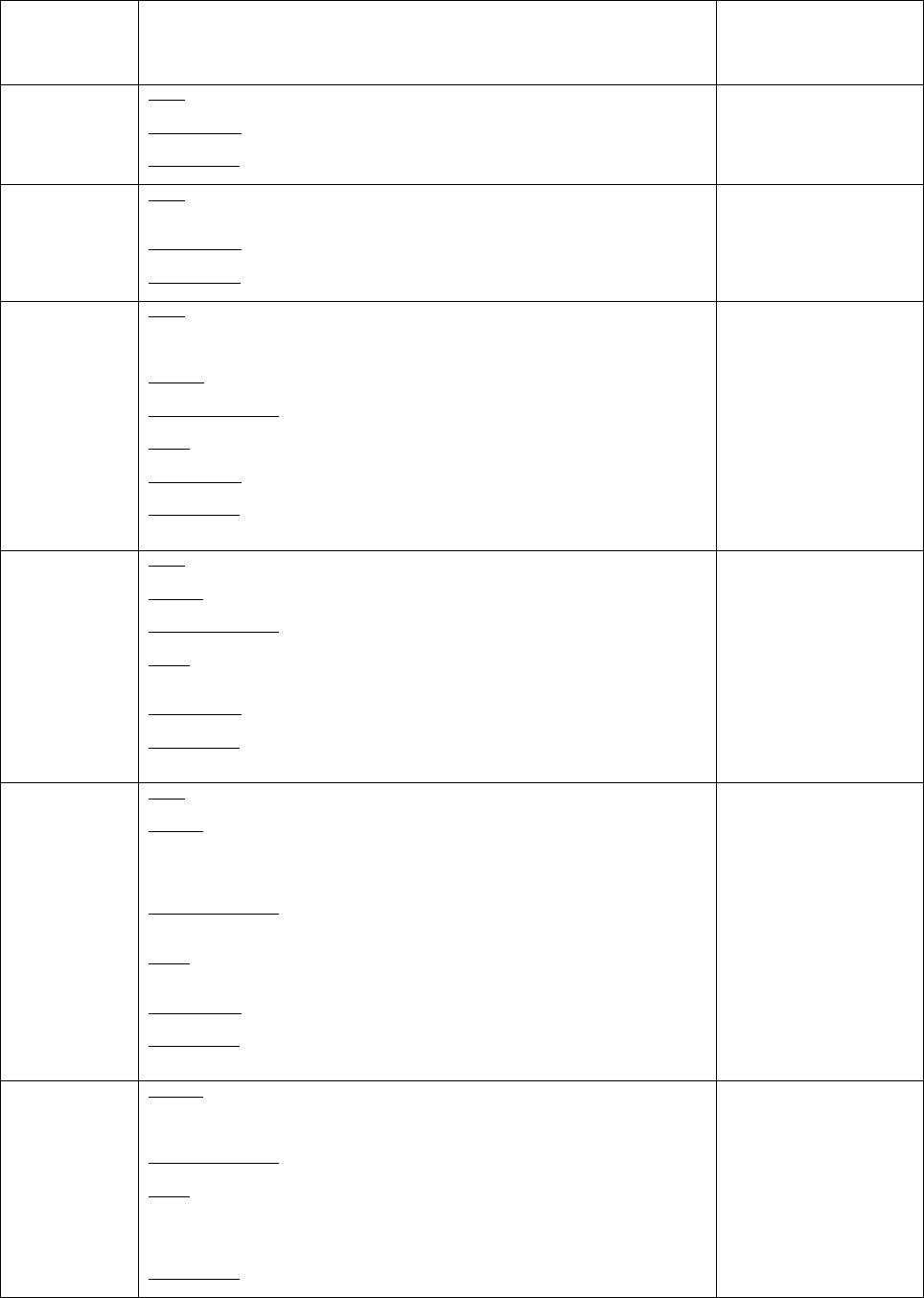
2. The three global HBC lists defined by WHO for 2016–2020
Following advice provided at the WHO STAG-TB meeting in 2015, the Global TB Programme finalized the
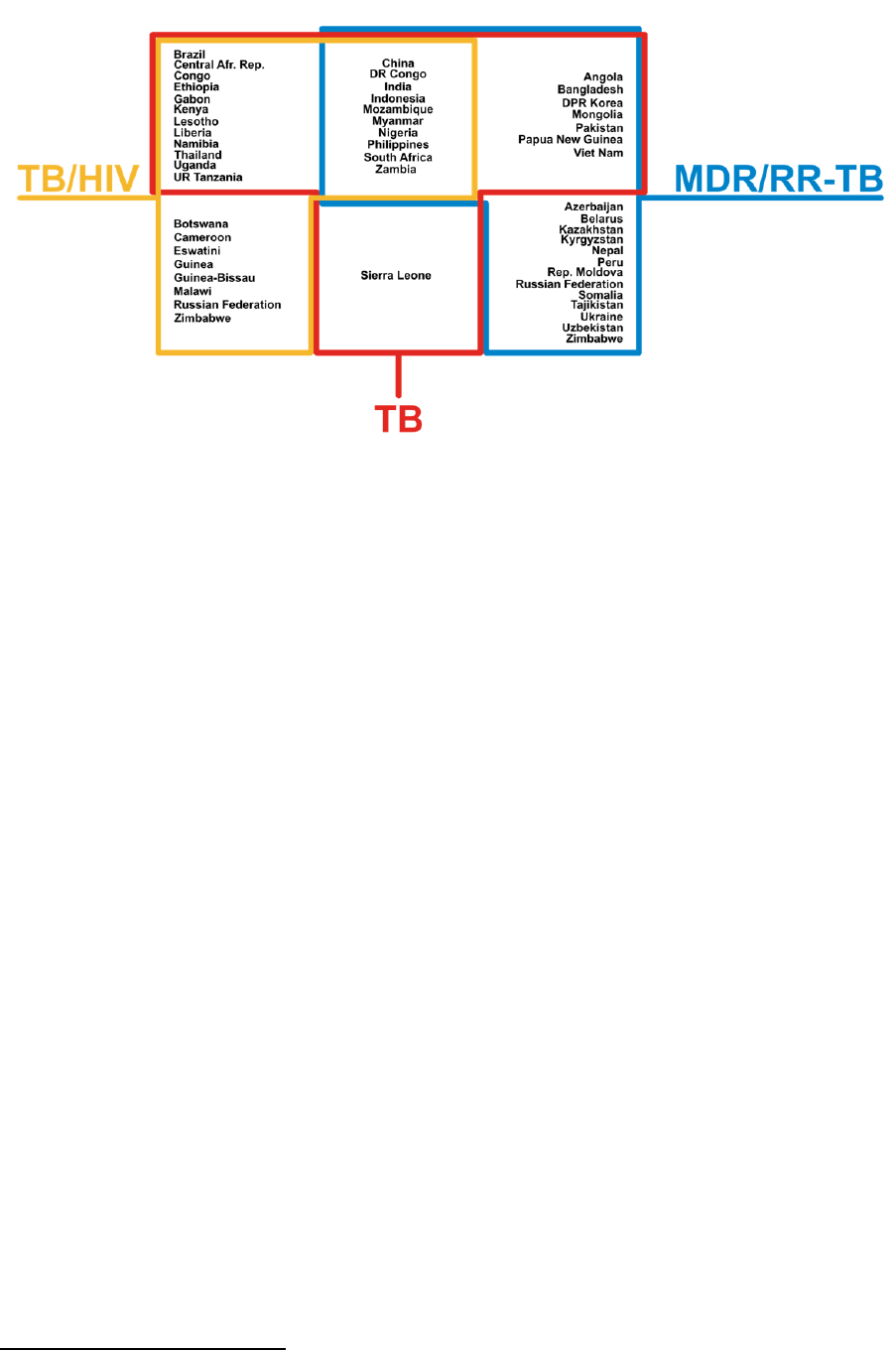
three global HBC lists to be used by WHO during the period 2016–2020. These are shown in Fig. 1 and
Table 1.
The minimum thresholds for the annual estimated numbers of cases that were used for countries included in
the lists on the basis of their incidence rates per 100 000 population per year were defined as 10 000 per year
for TB, and 1000 per year for TB/HIV and MDR-TB. Given overlap, the lists included a total of 48 countries
and 14 countries (see central diamond in the figure) were in all three lists.
Fig. 1: The three global HBC lists for TB, TB/HIV and MDR-TB used by WHO during the period
2016–2020, and their areas of overlap
4
See the report of the STAG-TB meeting in 2015 (pp8), available at
https://www.who.int/tb/advisory_bodies/stag_tb_report_2015.pdf?ua=1
4
Table 1: The three global lists of high burden countries for TB, TB/HIV and MDR-TB used by WHO during the period 2016–2020
Countries are listed alphabetically (not in order of their number of incident cases in absolute terms or per capita)
List
The 30 high TB burden countries
The 30 high TB/HIV burden countries
The 30 high MDR-TB burden countries
Purpose and
target audience
To provide a focus for global action on TB in the countries
where progress is most needed to achieve End TB Strategy
and SDG targets and milestones, to help build and sustain
national political commitment and funding in the countries
with the highest burden in terms of absolute numbers or
severity, and to promote global monitoring of progress in a
well-defined set of countries.
To provide a focus for global action on HIV-associated TB
in the countries where progress is most needed to achieve
End TB Strategy, UNAIDS and SDG targets and
milestones, to help build and sustain national political
commitment and funding in the countries with the highest
burden in terms of absolute numbers or severity, and to
promote global monitoring of progress in a well-defined
set of countries.
To provide a focus for global action on the MDR-TB crisis in
the countries where progress is most needed to achieve End
TB Strategy targets and milestones, to help build and sustain
national political commitment and funding in the countries
with the highest burden in terms of absolute numbers or
severity, and to promote global monitoring of progress in a
well-defined set of countries.
Definition
The 20 countries with the highest estimated numbers of
incident TB cases, plus the top 10 countries with the highest
estimated TB incidence rate that are not in the top 20 by
absolute number (threshold, >10 000 estimated incident TB
cases per year).
The 20 countries with the highest estimated numbers of
incident TB cases among people living with HIV, plus the
top 10 countries with the highest estimated TB/HIV
incidence rate that are not in the top 20 by absolute number
(threshold, >1000 estimated incident TB/HIV cases per
year).
The 20 countries with the highest estimated numbers of
incident MDR/RR-TB cases, plus the top 10 countries with
the highest estimated MDR/RR-TB incidence rate that are not
in the top 20 by absolute number (threshold, >1000 estimated
incident MDR-TB cases per year).
Countries in the
list, based on 2014
estimates of the
incidence of TB,
HIV-associated
TB and MDR-TB
published in the
2015 WHO global
TB report
The top 20 by estimated
absolute number (in
alphabetical order):
Angola
Bangladesh
Brazil
China
Democratic People’s Republic
of Korea
Democratic Republic of Congo
Ethiopia
India
Indonesia
Kenya
Mozambique
Myanmar
Nigeria
Pakistan
Philippines
Russian Federation
South Africa
Thailand
United Republic of Tanzania
Viet Nam
The additional 10 by
estimated incidence rate
per 100 000 population
per year and with a
minimum number of
10 000 cases per year (in
alphabetical order):
Cambodia
Central African Republic
Congo
Lesotho
Liberia
Namibia
Papua New Guinea
Sierra Leone
Zambia
Zimbabwe
The top 20 by estimated
absolute number (in
alphabetical order):
Angola
Brazil
Cameroon
China
Democratic Republic of Congo
Ethiopia
India
Indonesia
Kenya
Lesotho
Malawi
Mozambique
Myanmar
Nigeria
South Africa
Thailand
Uganda
United Republic of Tanzania
Zambia
Zimbabwe
The additional 10 by
estimated incidence rate
per 100 000 population
per year, and with a
minimum of 1000
incident cases per year
(in alphabetical order):
Botswana
Central African
Republic
Chad
Congo
Ghana
Guinea-Bissau
Liberia
Namibia
Papua New Guinea
Swaziland
The top 20 by estimated
absolute number (in
alphabetical order):
Bangladesh
China
Democratic People’s Republic
of Korea
Democratic Republic of Congo
Ethiopia
India
Indonesia
Kazakhstan
Kenya
Mozambique
Myanmar
Nigeria
Pakistan
Philippines
Russian Federation
South Africa
Thailand
Ukraine
Uzbekistan
Viet Nam
The additional 10 by
estimated rate per 100 000
population per year, and
with a minimum of 1000
incident cases per year (in
alphabetical order):
Angola
Azerbaijan
Belarus
Kyrgyzstan
Papua New Guinea
Peru
Republic of Moldova
Somalia
Tajikistan
Zimbabwe
Share of global
incidence in 2014
83%
3%
84%
5%
80%
5%
Lifetime of list
5 years
(review criteria and included countries in 2020).
5 years
(review criteria and included countries in 2020).
5 years
(review criteria and included countries in 2020).

5
Since the definition of the three new global HBC lists, WHO has given specific attention to the 30 high TB
burden countries in its monitoring of the status of the TB epidemic and progress in implementation and
financing of response efforts. For example, in the 2016, 2017, 2018, 2019 and 2020 editions of WHO’s
Global TB Report, the major chapters included many graphs and tables that focused on or gave particular
attention to the 30 high TB burden countries. Where estimates of disease burden and assessment of progress
in the response were for HIV-associated TB or MDR/RR-TB specifically, these reports gave specific
attention to countries in the other two lists. Infographic-style profiles for the 48 countries in at least one of
the three lists have been produced since 2018, and from 2015–2019 Annex 2 of the report provided a two-
page profile for each of the 30 high TB burden countries (in 2020, these profiles were moved to a Global TB
Report app and are also available online, along with identical profiles for all other countries).
Other examples of how WHO has given specific attention to HBCs at global level include:
• End TB Strategy Summits. These have been held annually since 2016, bringing together participants
from the 30 high TB burden countries and representatives from a range of technical and financial
partners to discuss the status of progress and specific high-priority topics.
• High-level dialogue. In 2019, the Director-General wrote to the Heads of State of the 48 countries
included in at least one of the 3 HBC lists (Fig. 1) to urge accelerated action to reach global TB
targets. This was done in follow-up to the first UN high-level meeting on TB held in September
2018. High-level missions to countries by senior WHO leadership have prioritized high TB burden
countries.
• The DG Flagship Initiative Find.Treat.All #EndTB. This has given particular attention to high TB
burden countries.
• Advocacy efforts. In follow-up to the UN high-level meeting on TB, a new campaign “Race to End
TB” was launched in high TB burden countries.
3. The three global HBC lists to be used by WHO in the period 2021–2025
The redesign of WHO global lists of HBCs for the period 2016–2020 followed an extensive consultation
process and no concerns with the criteria or the lists were expressed by Member States to WHO during this
period. Following consultations across the WHO TB network (including all WHO Regional Offices) in 2020
and with WHO’s current STAG-TB in February 2021,
5
three updated lists will used in the period 2021–2025.
The updated lists have been defined using the same criteria as those agreed in 2015 combined with the
latest estimates (for 2019) of the incidence of TB, HIV-associated TB and MDR/RR-TB published by
WHO in the Global Tuberculosis Report 2020. The new lists are shown in Fig. 2 and Table 2.
The changes compared with the previous lists for 2016–2020 (Fig. 1, Table 1) can be summarized as follows:
The 30 high TB burden countries – 3 new entries and 3 exits
• Gabon, Mongolia and Uganda added.
• Cambodia, the Russian Federation and Zimbabwe removed.
The 30 high TB/HIV burden countries – 4 new entries and 4 exits
• Gabon, Guinea, Philippines and the Russian Federation added.
• Angola, Chad, Ghana and Papua New Guinea removed.
The 30 high MDR/RR-TB burden countries - 3 new entries and 3 exits
• Mongolia, Nepal and Zambia added.
• Ethiopia, Kenya and Thailand removed.
Overall, three countries will no longer appear in a global HBC list: Cambodia, Chad and Ghana.
Four countries will be new inclusions in a global HBC list: Gabon, Guinea, Mongolia and Nepal.
Graphical illustrations of the estimates of incidence from which the top 20 and top 10 are identified are
provided in Appendix 1.
5
The current membership is 15 people serving in an individual capacity, none of whom were part of the group in 2015.
6
Table 2: The global lists of high burden countries for TB, TB/HIV and MDR/RR-TB to be used by WHO in the period 2021–2025
The lists are based on the same criteria as those used in 2015, combined with the latest (2019) estimates of the incidence of TB, HIV-associated TB and MDR/RR-TB published in WHO’s
Global Tuberculosis Report 2020
Countries are listed alphabetically (not in order of their number of incident cases in absolute terms or per capita)
List
The 30 high TB burden countries
The 30 high TB/HIV burden countries
The 30 high MDR/RR-TB burden countries
Purpose and target
audience
To provide a focus for global action on TB in the countries
where progress is most needed to achieve the targets and
milestones set in the WHO End TB Strategy, the political
declaration of the UN high-level meeting on TB held in 2018
and the SDGs, to help build and sustain national political
commitment and funding in the countries with the highest
burden in terms of absolute numbers or severity, and to
promote global monitoring of progress in a well-defined set of
countries.
To provide a focus for global action on HIV-associated TB in
the countries where progress is most needed to achieve targets
and milestones set in the WHO End TB Strategy, the political
declaration of the UN high-level meeting on TB held in 2018,
the UNAIDS global strategy for HIV/AIDS and the SDGs, to
help build and sustain national political commitment and
funding in the countries with the highest burden in terms of
absolute numbers or severity, and to promote global
monitoring of progress in a well-defined set of countries.
To provide a focus for global action on the public health
crisis of drug-resistant TB in the countries where progress
is most needed to achieve targets and milestones set in the
WHO End TB Strategy and the political declaration of the
UN high-level meeting on TB held in 2018, to help build
and sustain national political commitment and funding in
the countries with the highest burden in terms of absolute
numbers or severity, and to promote global monitoring of
progress in a well-defined set of countries.
Definition
The 20 countries with the highest estimated numbers of
incident TB cases, plus the top 10 countries with the highest
estimated TB incidence rate that are not in the top 20 by
absolute number (threshold, >10 000 estimated incident TB
cases per year).
The 20 countries with the highest estimated numbers of
incident TB cases among people living with HIV, plus the top
10 countries with the highest estimated TB/HIV incidence rate
that are not in the top 20 by absolute number (threshold, >1000
estimated incident TB/HIV cases per year).
The 20 countries with the highest estimated numbers of
incident MDR/RR-TB cases, plus the top 10 countries with
the highest estimated MDR/RR-TB incidence rate that are
not in the top 20 by absolute number (threshold, >1000
estimated incident MDR/RR-TB cases per year).
Countries in the
list, based on 2019
estimates of the
incidence of TB,
HIV-associated TB
and MDR/RR-TB
published in the
2020 WHO global
TB report
The top 20 by estimated absolute
number (in alphabetical order):
Angola
Bangladesh
Brazil
China
Democratic People’s Republic
of Korea
Democratic Republic of Congo
Ethiopia
India
Indonesia
Kenya
Mozambique
Myanmar
Nigeria
Pakistan
Philippines
South Africa
Thailand
Uganda
United Republic of Tanzania
Viet Nam
The additional 10 by
estimated incidence rate
per 100 000 population
per year and with a
minimum number of
10 000 cases per year (in
alphabetical order):
Central African Republic
Congo
Gabon
Lesotho
Liberia
Mongolia
Namibia
Papua New Guinea
Sierra Leone
Zambia
The top 20 by estimated absolute
number (in alphabetical order):
Brazil
Cameroon
China
Democcratic Republic of Congo
Ethiopia
India
Indonesia
Kenya
Malawi
Mozambique
Myanmar
Nigeria
Philippines
Russian Federation
South Africa
Thailand
Uganda
UR Tanzania
Zambia
Zimbabwe
The additional 10 by
estimated incidence rate
per 100 000 population
per year, and with a
minimum of 1000 incident
cases per year (in
alphabetical order):
Botswana
Central African Republic
Congo
Eswatini
Gabon
Guinea
Guinea-Bissau
Lesotho
Liberia
Namibia
The top 20 by estimated
absolute number (in
alphabetical order):
Angola
Bangladesh
China
Democratic People’s
Republic of Korea
Democratic Republic of Congo
India
Indonesia
Kazakhstan
Mozambique
Myanmar
Nigeria
Pakistan
Peru
Philippines
Russian Federation
Somalia
South Africa
Ukraine
Uzbekistan
Viet Nam
The additional 10 by
estimated rate per 100
000 population per year
and with a minimum of
1000 incident cases per
year (in alphabetical
order):
Azerbaijan
Belarus
Kyrgyzstan
Mongolia
Nepal
Papua New Guinea
Republic of Moldova
Tajikistan
Zambia
Zimbabwe
Share of global
incidence in 2019
84%
2.3%
83%
5.3%
86%
3.7%
Lifetime of list
5 years
(review criteria and included countries in 2025).
5 years
(review criteria and included countries in 2025).
5 years
(review criteria and included countries in 2025).
7
Fig. 2: The three global HBC lists for TB, TB/HIV and MDR/RR-TB to be used by WHO
during the period 2021–2025, and their areas of overlap
Following feedback on earlier versions of this document, the Global TB Programme will give continue
to give specific attention to the countries that are exiting the global list of high TB burden countries
(Cambodia, the Russian Federation, Zimbabwe), considering them as part of a “global TB watchlist”.
6
It should be highlighted that the context of the COVID-19 pandemic was considered prior to finalizing
the updated global HBC lists. In particular, an assessment of whether the impact of the pandemic on
TB incidence could plausibly affect the countries included in each list was done. Based on this analysis,
it was concluded that it was unlikely that the COVID-19 pandemic would change the countries included
in each list. Further details are available from the Global TB Programme upon request. An additional
justification (as commented during the review by STAG-TB) is that it will take time for concrete data
(as opposed to modelling projections) about the impact of COVID-19 on TB incidence to become
available, such that it is preferable to proceed with the updating of global HBC lists based on the
evidence already available.
It is also worth noting that future editions of the WHO global TB report will include a tabular
categorization or graphical illustration of all countries in terms of estimated TB incidence per 100 000
population per year. This will be updated each year (in contrast to the lifetime of five years for the
global HBC lists) and used to highlight countries that have made progress in terms of moving from one
category to a lower one, as well as to give some attention to low-incidence countries. A tabular
classification based on estimates of TB incidence per 100 000 population per year is provided in
Appendix 2. Such a classification and its updating on an annual basis was unanimously supported
during the STAG-TB review of an earlier version of this document in February 2021.
6
The Global TB Programme will also consider whether it would be useful to flag countries that are of particular concern (for
example based on evidence about the impact of the COVID-19 pandemic, or based on evidence of an increasing TB
incidence rate) via this concept of a global watchlist, during the period up to the next update of global HBC lists.

8
4. Complementing global HBC lists with regional priority lists
In line with the STAG-TB recommendation provided in 2015 (p3), additional countries can be given
priority attention at regional level.
Three WHO regional offices currently use regional priority lists for TB:
• Region of the Americas: There are 12 priority countries out of a total of 35 WHO Member
States in the region. They are defined as countries with an estimated absolute number of
incident cases of more than 10 000 per year and an incidence rate of more than 45 per 100 000
population per year. The priority countries are Argentina, Bolivia, Brazil, Colombia,
Dominican Republic, El Salvador, Guyana, Haiti, Mexico, Panama, Peru and Venezuela.
• European Region: There are 18 priority countries out of a total of 55 in the region. They are
defined as the countries that account for 85% of the regional TB burden and 99% of the regional
MDR/RR-TB burden (in terms of the absolute number of cases per year). The priority countries
are Armenia, Azerbaijan, Belarus, Bulgaria, Estonia, Georgia, Kazakhstan, Kyrgyzstan, Latvia,
Lithuania, the Republic of Moldova, Romania, the Russian Federation, Tajikistan, Turkey,
Turkmenistan, Ukraine and Uzbekistan.
• Western Pacific Region: There are currently seven priority countries out of a total of 36
countries and territories in the region. They are Cambodia, China, Lao People’s Democratic
Republic, Mongolia, Papua New Guinea, Philippines and Viet Nam, which collectively account
for >95% of the regional TB burden (in terms of the absolute number of cases per year). This
list is also being updated in 2021, to include the top 5 countries in terms of absolute numbers
of cases and the top 5 additional countries in terms of incidence per 100 000 population per
year (applying a threshold of at least 100 cases per year). The priority countries are Cambodia,
China, Kiribati, Lao People’s Democratic Republic, Marshall Islands, Micronesia, Mongolia,
Papua New Guinea, Philippines and Viet Nam. Both the current and updated lists ensure that
Cambodia, while exiting the global TB HBC list, is still prioritized at regional level.
As in the STAG-TB review of 2015, feedback received during the review by STAG-TB in February
2021 included that it would be preferable to ensure that the criteria used to define regional priority lists
are aligned as much as possible with the criteria used to define the global HBC lists. It was also
acknowledged that some region-specific customization may be necessary, for example due to the
varying number of Member States among WHO regions (which ranges from 11 in the South-East Asia
Region to 55 in the European Region).
9
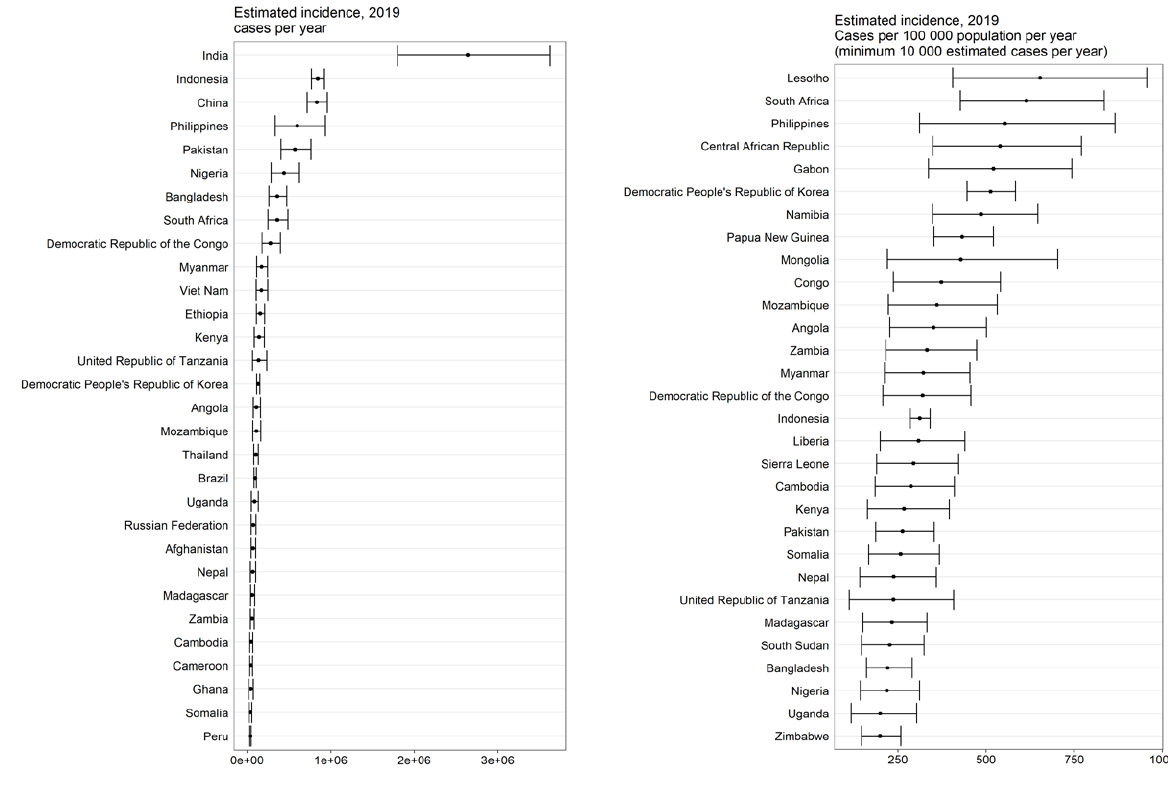
Appendix 1: Estimates of the incidence of TB, HIV-associated TB and MDR/RR-TB in 2019
Fig. A1: Top 30 countries in terms of absolute numbers and rates: TB, based on incidence estimates for 2019
10
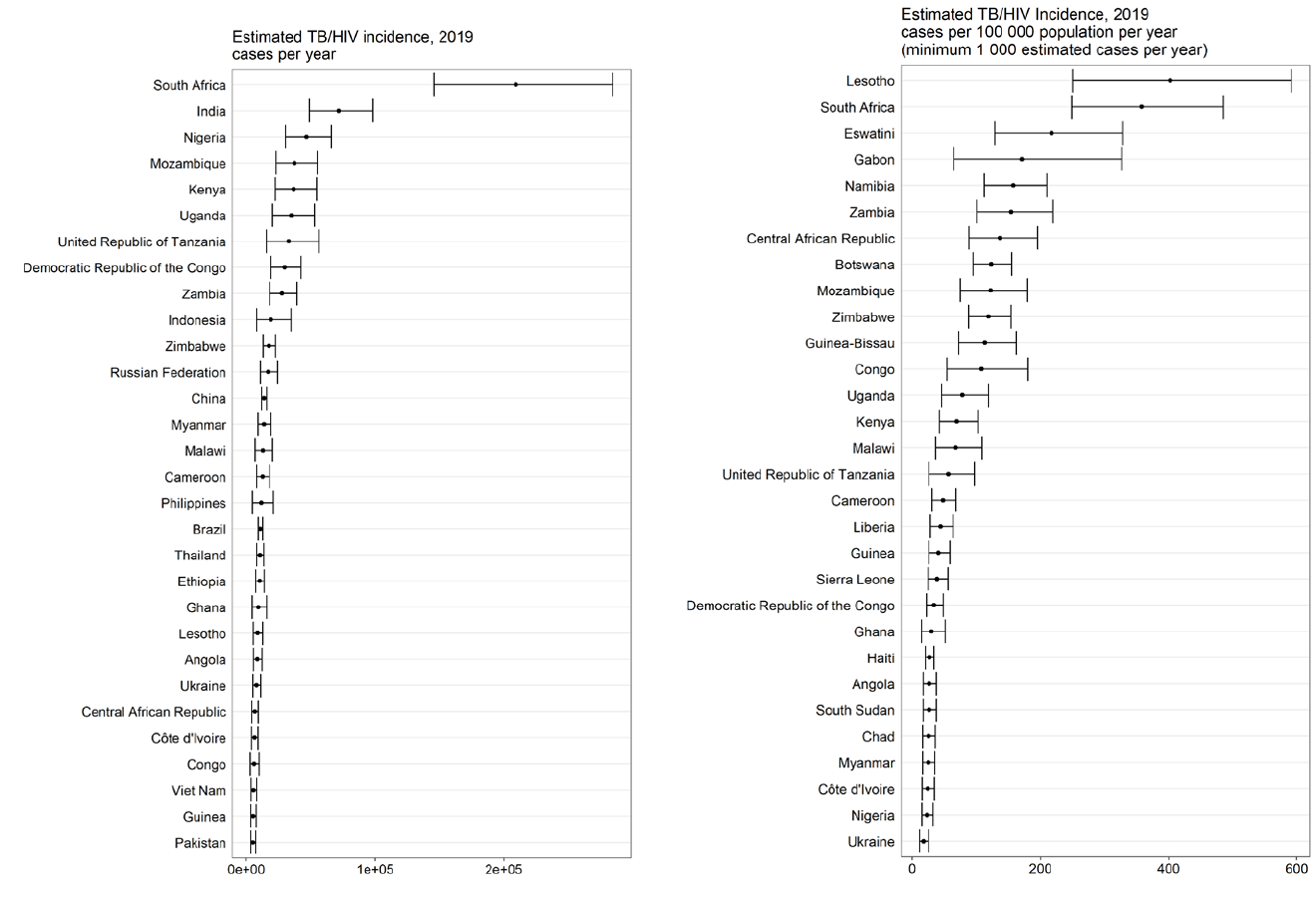
Fig. A2: Top 30 countries in terms of absolute numbers and rates: TB/HIV, based on incidence estimates for 2019
11
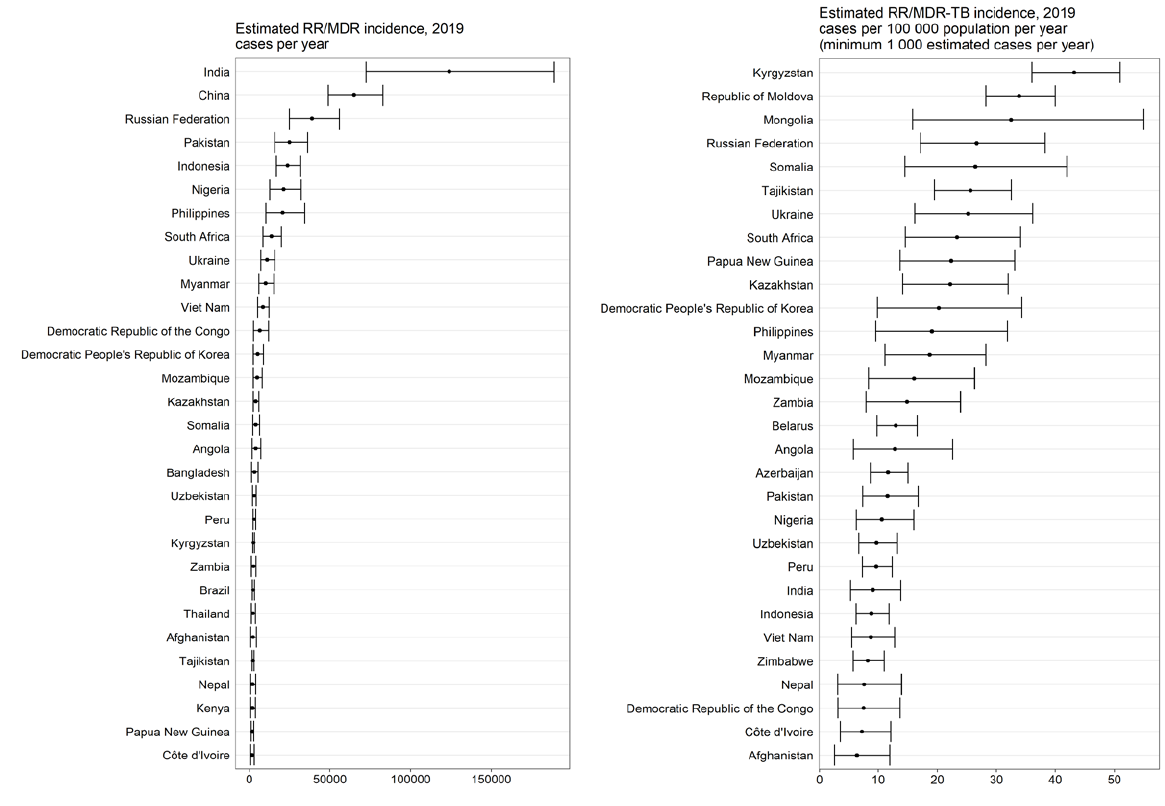
Fig. A3: Top 30 countries in terms of absolute numbers and rates: MDR/RR-TB, based on incidence estimates for 2019
12
Appendix 2. Categorization of all countries based on TB incidence per 100 000 population
per year
In 2015, it was noted in the final version of the WHO discussion paper on global HBC lists that:
“Several reviewers of earlier drafts of this document also commented that it would be very
helpful to categorize countries in terms of their TB burden (e.g. high, medium, low, using for
example the TB incidence rate per capita), and to present… (this categorization) in annual
global TB reports. Such a categorization would be all-inclusive and also allow progress to be
illustrated as countries graduate from one category to another.”
7
A tabular or graphical categorization will be included for the first time in the 2021 edition of the WHO
global TB report, and subsequently updated on an annual basis (in contrast to the global HBC lists that
have a lifetime of 5 years). Countries that have transitioned from one category to another in the most
recent year will be highlighted.
Following consultations with regional offices, the categorization that will be used is based on TB
incidence rates, as follows:
• severely endemic (≥500 new and relapse cases per 100 000 population per year);
• highly endemic (300–499 new and relapse cases per 100 000 population per year);
• endemic (100–299 new and relapse cases per 100 000 population per year);
• upper-moderate (50–99 new and relapse cases per 100 000 population per year);
• lower-moderate (10–49 new and relapse cases per 100 000 population per year);
• low (<10 new and relapse cases per 100 000 population per year).
This categorization is aligned with a categorization included in the WHO Western Pacific Regional
Office’s (WPRO) Regional framework for TB, 2021–2030.
The “low-incidence” category corresponds to the group of countries considered in the TB elimination
framework published by WHO in 2014.
8
This framework set out how the End TB Strategy could be
adapted in countries with an incidence of <10 per 100 000 population per year,
9
with the aim of making
progress to “pre-elimination” (defined as <1 incident case per 100 000 population per year) and then to
elimination of TB as a public health problem (defined as <1 incident case per million population per
year). The low-incidence category can also be used to inform decisions about which countries to
consider for inclusion in global or regional initiatives and projects relate to “TB elimination”. For
example, these could include countries in the category of <10 incident cases per 100 000 population per
year as well a few countries with best estimates that are around the threshold of 10 incident cases per
100 000 population per year (e.g. Costa Rica). The WHO Global TB Programme is updating the WHO
TB Elimination Framework in 2021.
Table A2.1 illustrates how countries would be categorized according to estimates of TB incidence for
2019 that were published in the Global Tuberculosis Report 2020, and the number of countries and the
collective share of the global TB burden (in terms of the absolute number of incident cases) accounted
for by each category.
7
Use of high burden country lists for TB by WHO in the post-2015 era. Discussion paper initially prepared in April 2015 to
facilitate feedback, and finalized after the June 2015 meeting of WHO’s Strategic and Technical Advisory Group for TB
(STAG-TB). See pp6. Available at:
https://www.who.int/tb/publications/global_report/high_tb_burdencountrylists2016-
2020.pdf
8
Towards tuberculosis elimination: an action framework for low-incidence countries. WHO, 2014. Available at
https://www.who.int/tb/publications/elimination_framework/en/
9
The framework used the equivalent definition of <100 incident cases per million population per year.
13
Table A2.1. Epidemiological categorization of countries and territories based on incidence per 100 000
population per year in 2019
Incidence category
Countries included, by WHO region
Number of countries and
category share (%) of the
total estimated number of
incident TB cases globally in
2019
Severely endemic
(≥500 new and
relapse cases per
100 000 population
per year)
Africa
Central African Republic, Gabon, Lesotho, South Africa
South-East Asia
Democratic People's Republic of Korea
Western Pacific
Philippines
n=6
11%
Highly endemic
(300–499 new and
relapse cases per
100 000 population
per year)
Africa
Angola, Congo, Democratic Republic of the Congo, Eswatini, , Guinea-Bissau, Liberia,
Mozambique, Namibia, Zambia
South-East Asia
Indonesia, Myanmar, Timor-Leste
Western Pacific
Kiribati, Marshall Islands, Mongolia, Papua New Guinea
n=16
17%
Endemic
(100–299 new and
relapse cases per
100 000 population
per year)
Africa
Botswana, Burundi, Cameroon, Chad, Côte d'Ivoire, Equatorial Guinea, Ethiopia, Gambia,
Ghana, Guinea, Kenya, Madagascar, Malawi, Nigeria, Sao Tome and Principe, Senegal, Sierra
Leone, South Sudan, Uganda, United Republic of Tanzania, Zimbabwe
Americas
Bolivia (Plurinational State of), Haiti, Peru
Eastern Mediterranean
Afghanistan, Djibouti, Pakistan, Somalia
Europe
Greenland, Kyrgyzstan
South-East Asia
Bangladesh, Bhutan, India, Nepal, Thailand
Western Pacific
Cambodia, Lao People's Democratic Republic, Micronesia (Federated States of), Nauru, Northern
Mariana Islands, Tuvalu, Viet Nam
n=42
55%
Upper-moderate
(50-99 new and
relapse cases per
100 000 population
per year)
Africa
Algeria, Benin, Eritrea, Mali, Mauritania, Niger, Rwanda
Americas
El Salvador, Guyana
Eastern Mediterranean
Libya, Morocco, Sudan
Europe
Azerbaijan, Georgia, Kazakhstan, Republic of Moldova, Romania, Russian Federation,
Tajikistan, Ukraine, Uzbekistan
South-East Asia
Sri Lanka
Western Pacific
Brunei Darussalam, China, China Hong Kong SAR, China Macao SAR, Fiji, Guam, , Malaysia,
Republic of Korea, Solomon Islands
n=31
12%
Lower-moderate
(10-49 new and
relapse cases per
100 000 population
per year)
Africa
Burkina Faso, Cabo Verde, Comoros, Mauritius, Seychelles, Togo
Americas
Anguilla, Argentina, Bahamas, Belize, Brazil, Chile, Colombia, Costa Rica, Dominica,
Dominican Republic, Ecuador, Guatemala, Honduras, Mexico, Nicaragua, Panama, Paraguay,
Sint Maarten (Dutch part), Suriname, Trinidad and Tobago, Turks and Caicos Islands, Uruguay,
Venezuela (Bolivarian Republic of)
Eastern Mediterranean
Bahrain, Egypt, Iran (Islamic Republic of), Iraq, Kuwait, Lebanon, Qatar, Saudi Arabia, Syrian
Arab Republic, Tunisia, Yemen
Europe
Albania, Armenia, Belarus, Bosnia and Herzegovina, Bulgaria, Estonia, Latvia, Lithuania,
Malta, Montenegro, North Macedonia, Poland, Portugal, Serbia, Turkey, Turkmenistan
South-East Asia
Maldives
Western Pacific
Cook Islands, French Polynesia, Japan, Palau, Samoa, Singapore, Tokelau, Tonga, Vanuatu,
Wallis and Futuna Islands
n=67
3%
Low
(<10 new and
relapse cases per
100 000 population
per year)
Americas
Antigua and Barbuda, Aruba, Barbados, Bermuda,
British Virgin Islands, Canada, Cayman
Islands, Cuba, Curaçao, Grenada, Jamaica, Montserrat, Puerto Rico, Saint Kitts and Nevis, Saint
Lucia, Saint Vincent and the Grenadines, United States of America
Eastern Mediterranean
Jordan, occupied Palestinian territory including east Jerusalem, Oman, United Arab Emirates
Europe
Andorra, Austria, Belgium, Croatia, Cyprus, Czechia, Denmark, Finland, France, Germany,
Greece, Hungary, Iceland, Ireland, Israel, Italy, Luxembourg, Monaco, Netherlands, Norway, San
Marino,
Slovakia, Slovenia, Spain, Sweden, Switzerland, United Kingdom of Great Britain and
Northern Ireland
Western Pacific
American Samoa, Australia, New Caledonia, New Zealand, Niue
n=53
0.5%

14
